Osteoarthritis: A Physio Guide!
Overview of Osteoarthritis
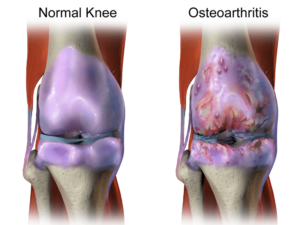
Osteoarthritis (OA) is the most common form of arthritis, affecting millions of people worldwide. It is a degenerative joint disease characterized by the breakdown of cartilage in the joints, leading to pain, stiffness, and reduced mobility. OA typically affects weight-bearing joints such as the knees, hips, and spine, but it can also involve other joints such as the hands and feet. While OA is more common in older adults, it can also affect younger individuals, especially those with a history of joint injury or overuse.
Detailed Diagnosis of Osteoarthritis
- Physical Examination:
- Joint tenderness and swelling
- Crepitus (crackling or grating sensation)
- Decreased range of motion
- Joint instability
- Imaging Studies:
- X-rays: To assess joint damage, including cartilage loss, bone spurs, and joint space narrowing.
- MRI (Magnetic Resonance Imaging): To visualize soft tissues such as cartilage and ligaments in greater detail.
- Laboratory Tests:
- Blood tests: To rule out other types of arthritis, such as rheumatoid arthritis.
Role of Physiotherapy in Osteoarthritis:
Physiotherapy plays a crucial role in the management of osteoarthritis, aiming to reduce pain, improve joint function, and enhance quality of life. Physiotherapists employ a variety of techniques and interventions tailored to the individual needs of patients.
Detailed Assessment of Osteoarthritis with Special Tests in Physiotherapy
- Gait Analysis: To assess walking pattern and detect any abnormalities or asymmetries.
- Muscle Strength Testing: To evaluate muscle weakness or imbalance around the affected joint.
- Range of Motion Measurement: To determine the extent of joint stiffness and limitations in movement.
- Functional Mobility Assessment: To assess the patient’s ability to perform daily activities such as walking, climbing stairs, and getting up from a chair.
Detailed Applied Physiotherapy Treatment
Exercise Therapy:
- Quadriceps Strengthening: Straight leg raises, seated leg extensions, and wall squats improve muscle strength around the knee joint.
- Hamstring Stretching: Supine hamstring stretch, standing hamstring stretch, and seated hamstring stretch to increase flexibility and reduce joint stiffness.
- Aerobic Exercises: Walking, cycling, swimming, and aquatic exercises to improve cardiovascular fitness and overall function.
- Hip Flexor Stretch: Kneel on one knee, keeping the other foot flat on the ground, and gently push the hips forward until a stretch is felt in the front of the hip.
- Calf Stretch: Stand facing a wall with one foot forward and one foot back, keeping both heels on the ground, and lean forward, bending the front knee while keeping the back knee straight to stretch the calf muscles.
- Gluteal Strengthening: Side-lying hip abduction, clamshell exercises, and bridges to strengthen the muscles around the hip joint.
Electrotherapy Treatment:
- Transcutaneous Electrical Nerve Stimulation (TENS): To relieve pain by stimulating nerves and blocking pain signals.
- Ultrasound Therapy: To promote tissue healing and reduce inflammation through the application of high-frequency sound waves.
- Interferential Current (IFC) Therapy: IFC therapy uses medium-frequency electrical currents to relieve pain and stimulate muscle contractions, aiding in pain management and muscle rehabilitation.
Electrotherapy modalities offer non-invasive pain relief and can complement exercise therapy to improve treatment outcomes.
Home Exercises
- Advantages of Home Exercises:
- Convenient and accessible
- Can be performed at any time
- Empowers patients to take control of their own rehabilitation
- Examples of Home Exercises:
- Knee Flexion and Extension: Sitting on a chair, slowly bend and straighten the affected knee.
- Hip Abduction and Adduction: Lie on your side and lift the top leg upward and downward.
- Wall Squats: Stand with your back against a wall and lower yourself into a seated position, then return to standing.
Prognosis
The prognosis for osteoarthritis varies depending on factors such as the severity of joint damage, the effectiveness of treatment, and the patient’s overall health. While OA is a chronic condition with no cure, appropriate management strategies, including physiotherapy, can help alleviate symptoms and improve function, allowing individuals to maintain an active and fulfilling lifestyle.
Conclusion
Osteoarthritis is a prevalent and debilitating condition that affects millions of people worldwide. However, with early diagnosis and comprehensive management, including physiotherapy interventions, individuals with OA can experience significant improvements in pain relief, joint function, and overall quality of life. By employing a multidisciplinary approach that addresses both the physical and psychological aspects of the disease, healthcare professionals can help patients effectively manage their symptoms and achieve better long-term outcomes.
