Heart Transplant Recovery: Your Path to Healing
Your heart transplant recovery is a journey filled with hope and challenges. Find support from loved ones and join transplant recipient groups. Set realistic goals and understand the changes ahead. Educate yourself about the procedure for empowerment. Adapt your diet and prioritize physical activity for a healthy recovery.

Someone’s heart is really struggling, and they need all the help they can get just to keep going. It’s a tough spot to be in, no doubt about it. But guess what? There’s a ray of hope shining through, and it’s called a heart transplant! Back in the day, the first tries at this were a bit rough. Sadly, the first patient didn’t make it very far. But hold onto your hats, because things have changed! With incredible advances in medicine and surgery, heart transplants have become a beacon of success. From the 90s onward, there’s been a surge in the number of transplants happening, and it’s not showing any signs of slowing down!
But here’s the kicker: There are more people in need of new hearts than there are hearts available. Can you believe it? Thankfully, though, experts have set some clear rules about who gets first dibs. This review is going to take us on a thrilling journey through it all—what those rules are, the different kinds of surgeries they perform, the awesome drugs people take afterward, and even some of the hurdles they might encounter along the way. Exciting, right?
Let’s buckle up and dive headfirst into this fascinating world of heart transplants!
Exploring Heart Transplant Procedures:
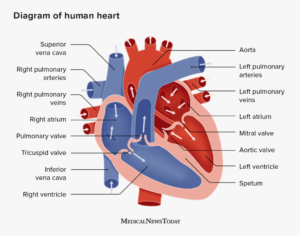
To grasp the intricacies of the transplant procedure, you need to delve into the anatomy and physiology of the heart and the major vessels in the mediastinum. In the history of transplantation, two main procedures have been identified:
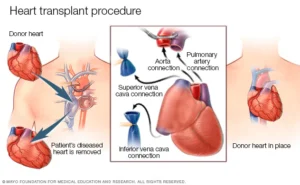
- First, there’s the ‘orthotopic heart transplant,’ where your heart is removed, and a donor’s heart is placed in your chest.
- Then, there’s the ‘heterotropic heart transplant,’ where your heart isn’t removed, and the donor heart is added to your chest alongside yours.
Understanding When to Consider a Heart Transplant:
To ensure timely placement on the transplant list, it’s crucial to recognize the indications for heart transplants. This ensures that patients can sustain themselves with inotropic support or mechanical assistance until a donor heart becomes available. However, it’s essential to rule out any contraindications before making a referral.
Indications for Urgent Referral in Chronic Heart Failure:
If you’re working in outpatient settings, consider referring the following categories of chronic heart failure patients for a heart transplant:

- Patients who, despite receiving guideline-directed medical therapy (GDMT), still experience significant symptoms during exertion, categorized as New York Heart Association class III or IV, or American College of Cardiology stage D patients.
- Patients who frequently require hospital readmissions due to exacerbations of heart failure, even with strict adherence to GDMT (two or more readmissions within 12 months),.
- Individuals experiencing worsening renal function attributed to cardiorenal syndrome.
- Those facing dose-limiting side effects like hypotension or contraindications such as renal failure are preventing the effective use of GDMT.
- Patients showing progressive deterioration in right ventricular function or increasing pulmonary artery pressure due to left heart failure.
- Individuals experiencing frequent episodes of ventricular arrhythmias persist despite receiving optimal drug therapy and electrophysiological interventions.
- Presence of other features such as anemia, weight loss, hyponatremia, or liver dysfunction attributable to heart failure.
Indications for Urgent Referral in Acute Heart Failure:
In inpatient settings, urgent referral for cardiac transplant is necessary for patients experiencing:

- Refractory cardiogenic shock despite receiving the maximum dose of inotropic treatment.
- Persistent cardiogenic shock despite undergoing percutaneous mechanical circulatory support.
- Failure of pulmonary edema to respond to diuretics, necessitates ventilation and positive pressure in the lungs.
- Intractable ventricular arrhythmias are unresponsive to medical treatment or electrophysiological procedures.
Heart Transplant Contraindications:
It’s disheartening that many patients with advanced heart failure, who meet the criteria for a heart transplant, might not be eligible due to various contraindications:
Active Infection:
Acute infections must be treated before considering transplantation. However, patients with well-controlled chronic infections like HIV, hepatitis C, and B, with undetectable titers and no end-organ damage, might still be considered.
Chronic Liver Disease (Cirrhosis):
This condition poses a contraindication.
Advanced Kidney Disease:
Patients with a glomerular filtration rate of less than 30 ml/min/1.73 m2 are not suitable candidates.
Recent Stroke or Symptomatic, Untreated Peripheral Vascular Disease:
Patients with these conditions are not eligible.
Uncontrolled diabetes mellitus:
Especially if it has led to end-organ damage.
Active Malignancy:
A discussion with oncologists is necessary to determine if transplantation is feasible.
Severe Lung Disease:
If the forced expiratory volume (FEV1) and forced vital capacity (FVC) are less than 50% predicted or if there is evidence of parenchymal lung disease.
Recent Pulmonary Embolism Requiring Anticoagulation:
Within the last 3 to 6 months.
Severe Pulmonary Hypertension (PH):
If pulmonary artery systolic pressure exceeds 60 mmHg and pulmonary vascular resistance exceeds 5 Wood units, and especially if PH is refractory to medical therapy,.
Psychosocial Factors:
Including lack of social support, disabling psychiatric illness, non-compliance with previous medical management, active smoking or drug use, and unwillingness to quit.
Morbid Obesity:
Defined as a body mass index greater than 35 kg/m2.
Multisystem Disease Requiring Other Transplant Procedures:
Such as renal, hepatic, or lung transplant.
Equipment and Personnel for Heart Transplantation:
The success of a heart transplant hinges on having the right equipment and skilled personnel in place:
Equipment:
- A well-preserved donor heart and a suitable recipient are the primary requirements.
- Cardiopulmonary bypass apparatus is essential during the procedure.
- Various surgical instruments, including surgical blades and saws for chest opening and dissection, clamps for retraction, cannulas for engaging major vessels, and sutures for anastomosis and chest closure, are needed.
Personnel:
- A team of assistant surgeons supports the highly trained cardiothoracic surgeon leading the procedure.
- A cardiac anesthesiologist administers general anesthesia, ensuring the recipient’s comfort and safety.
- A cohesive heart transplantation team comprising cardiac surgeons, cardiac anesthesiologists, cardiologists, perfusionists, and nursing staff, along with personnel coordinating organ transplantation, is essential.
- Adequate infrastructure, including a well-equipped operating room and an intensive care unit, is necessary.
Preparation of a Heart Transplant:
- Once a potentially suitable donor is confirmed, the recipient, after being prepared (shaved, washed with 4% chlorhexidine, and fasting), is taken to the operating room in coordination with the availability of the donor heart.
- The transplant registry selects an appropriate donor heart after matching.
- General anesthesia isn’t induced until the donor heart’s acceptability is confirmed.
- The recipient’s heart is removed before the donor heart becomes available to minimize ischemia time.
- Upon opening the recipient’s chest, the heart and surrounding structures are dissected and prepared for cardiopulmonary bypass.
- The timing of donor heart retrieval is carefully coordinated to minimize ischemia time.
- The entire surgery is performed under general anesthesia using cardiopulmonary bypass, transesophageal echocardiography, and multiple monitoring techniques, including Swan-Ganz catheters.
Implantation Techniques for Heart Transplantation:
Orthotopic Heart Transplantation:
This procedure, more commonly performed, involves the following steps:
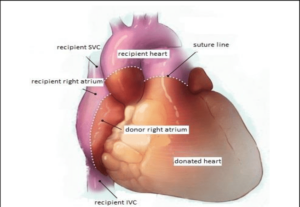
- Excision of the recipient’s heart, leaving the cuffs of the right and left atria intact.
- Transplantation of the donor’s heart involves connecting the donor and recipient’s right atrium to their respective cuffs, and similarly for the left atrium.
- Anastomosis of the donor’s aorta and pulmonary artery to the recipient’s corresponding vessels.
- Utilization of a bicaval technique, where the recipient’s right atrium is fully excised, and the recipient’s vena cavae are connected to the donor’s right atrium.
Heterotopic Heart Transplantation:
This procedure is rare and has been performed only a few times worldwide. It involves:
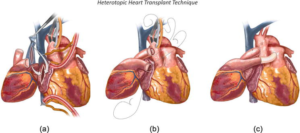
- Not excising the recipient’s heart.
- Transplanting the donor’s heart into the patient’s thoracic cavity.
- Making connections (anastomosis) between the donor and recipient atria.
- Connecting the donor’s aorta to the recipient’s aorta, and the donor’s pulmonary artery to the recipient’s pulmonary artery.
The following section provides a detailed description of the orthotopic heart transplant procedure.
Recipient Heart Excision:
- First, your chest is opened with a sternotomy and a pericardiotomy.
- The aorta and pulmonary veins are separated, while the superior and inferior vena cavae are mobilized and secured.
- Heparin is administered, and cannulas are placed in the aorta, superior vena cava, and inferior vena cava.
- With the donor heart arriving soon, cardiopulmonary bypass is initiated at a hypothermic temperature.
- Surgeons excise the left atrium to decompress the left heart, followed by excising the right atrium above the inferior vena cava.
- Both the aorta and pulmonary arteries are excised above the valves.
- The left atrial incision is extended into the appendage, excising it.
- The recipient’s heart is fully excised.
Donor’s Heart Preparation:
- The donor heart’s pulmonary veins are joined, and the left atrial cuff is trimmed to match the recipient’s.
- Inspection of the mitral valve and foramen ovale is conducted, and the great vessels (aorta and pulmonary artery) are excised.
Reperfusion and Completion:
- The great vessels are unclamped, a reperfusion of the heart.
- Reperfusion continues for at least 30 minutes while the heart rewarming process occurs.
- De-airing is performed to decompress the ventricles.
- You are slowly weaned off bypass.
- Mediastinal drains are placed, and protamine is administered to reverse heparin.
- Your chest is closed, and careful monitoring ensues.
Your Post-Transplant Journey: What to Expect and How to Thrive
- Your recovery post-heart transplant begins with transitioning from the intensive care unit to a standard hospital room, typically lasting one to two weeks, followed by continued monitoring from your transplant team.
- Vigilance for signs of rejection, such as shortness of breath or fever, remains crucial, with regular heart biopsies aiding in early detection.
- Consistent adherence to medication regimens, including immunosuppressants, is vital for preventing rejection and maintaining overall health.
- Lifestyle adjustments, like adopting a heart-healthy diet and staying physically active, support your recovery, while participation in cardiac rehabilitation programs can further enhance your cardiovascular health.
- By prioritizing self-care, staying connected with your medical team, and seeking support as needed, you’ll navigate this post-transplant period with resilience and determination, paving the way for a brighter, healthier future.
Heart Transplant Journey: Nurturing Your Well-being
- Feeling anxious or overwhelmed is common before and after a transplant.
- Seek support from loved ones and join transplant recipient groups.
- Set realistic goals and understand that life may change post-transplant.
- Educate yourself about the procedure to feel empowered.
- After a transplant, adapt your diet to maintain heart health.
- Consult with a dietitian for personalized dietary recommendations.
- Emphasize plant-based foods, lean meats, and heart-healthy fats.
- Stay hydrated and follow food safety guidelines.
- Regular exercise, tailored to your needs, is vital for physical and mental health post-transplant.
- Participate in cardiac rehabilitation to improve endurance, strength, and overall health.
As you embark on your heart transplant recovery journey, remember that you’re not alone. With the guidance of your medical team and the love of your support network, you’ll navigate the challenges ahead with strength and resilience. Each day is a step forward towards a brighter, healthier future. Embrace this journey with optimism and determination, knowing that the gift of life has opened doors to endless possibilities!
From struggling hearts to a new start,
Transplants heal, mending every part.

Pingback: Heart Transplant Evolution: From Pioneers to Modern Miracles -