Muscle Pain & Nerve Pain: An In-Depth Physio Perspective
Muscle pain & nerve pain are two common types of discomfort that affect a large portion of the population. While they may present with similar symptoms, their underlying causes, mechanisms, and treatments can be quite different. Understanding these differences is crucial for effective diagnosis and management.
This article will delve into the specifics of muscle pain and nerve pain, exploring their signs, symptoms, causes, mechanisms of action, differences, diagnostic approaches, and detailed physiotherapy treatments.
ANATOMY OF MUSCLE AND NERVE
Anatomy of Muscle:
- Muscle Fiber: The basic unit of muscle tissue, composed of myofibrils and surrounded by connective tissue.
- Fascicle: Bundle of muscle fibers surrounded by perimysium.
- Muscle Belly: The main body of the muscle, composed of multiple fascicles.
- Tendon: Connective tissue structure that attaches muscle to bone.
- Muscle Origin and Insertion: Points where the muscle attaches to bones or other structures.
- Blood Supply: Muscles receive blood through arteries, which deliver oxygen and nutrients, and veins, which remove waste products.
- Nerve Supply: Motor neurons innervate muscles, controlling voluntary and involuntary muscle contractions.

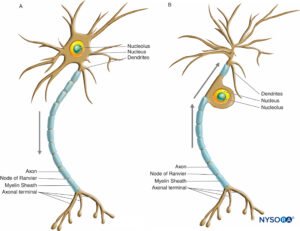
Anatomy of the Nerve:
- Neuron: A basic unit of the nervous system, consisting of a cell body, dendrites, and an axon.
- Nerve Fiber: Long, slender extension of a neuron, through which electrical impulses are transmitted.
- Nerve Bundle: A collection of nerve fibers surrounded by connective tissue.
- Nerve Trunk: Larger grouping of nerve bundles, often found in the limbs.
- Nerve Root: The point at which nerves emerge from the spinal cord.
- Nerve Plexus: A network of intersecting nerves, often found in regions such as the cervical or brachial plexus.
- Peripheral Nerves: Nerves that extend from the spinal cord to innervate muscles and transmit sensory information.
- Myelin Sheath: Fatty tissue that surrounds and insulates nerve fibers, speeding up signal transmission.
- Nodes of Ranvier: Gaps in the myelin sheath where nerve impulses are regenerated.
Microscopic Structure:
- Muscle: Myofibrils contain the contractile proteins actin and myosin, arranged in repeating units called sarcomeres.
- Nerve: Neurons consist of a cell body containing the nucleus, dendrites that receive signals, and an axon that transmits signals away from the cell body.
Ultrastructure:
- Muscle: Sarcomeres contain thick myosin filaments and thin actin filaments, which slide past each other during muscle contraction.
- Nerve: Axons are surrounded by a lipid-rich myelin sheath, which enhances signal conduction speed.
Functional Anatomy:
- Muscle: Responsible for generating force and producing movement through contraction and relaxation.
- Nerve: Transmit electrical impulses throughout the body, controlling muscle movement, sensation, and organ function.
What is Muscle Pain?
Muscle pain, also known as myalgia, refers to discomfort or pain originating from muscles. This type of pain can range from mild to severe and can be acute (short-term) or chronic (long-term). Muscle pain can result from various causes, including injury, overuse, tension, and certain medical conditions.

What is Nerve Pain?
Nerve pain, or neuropathic pain, arises from damage or dysfunction of the nerves themselves. Unlike muscle pain, which typically results from physical strain or injury, nerve pain is often associated with a malfunction in the nervous system. This type of pain can be sharp, burning, or shooting and can significantly affect the quality of life.

Signs, Symptoms, and Causes of Muscle Pain
Signs and Symptoms:
- Soreness or stiffness in the affected muscle
- Tenderness to touch
- Swelling or redness around the muscle
- Limited range of motion
- Muscle spasms or cramps
- Weakness in the affected area
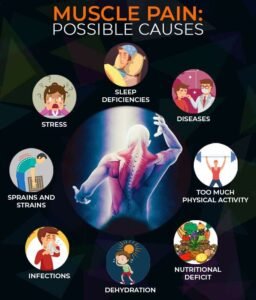
Causes:
- Injury: Strains, sprains, and tears are common causes of muscle pain. These injuries can occur due to accidents, falls, or sudden movements.
- Overuse: Repetitive activities, such as lifting heavy objects or engaging in high-intensity workouts, can lead to muscle fatigue and pain.
- Tension and Stress: Emotional stress and tension can cause muscle tightness, especially in the neck, shoulders, and back.
- Infections: Viral infections like influenza can cause generalized muscle pain.
- Medical Conditions: Conditions such as fibromyalgia, chronic fatigue syndrome, and myofascial pain syndrome can lead to persistent muscle pain.
Signs, Symptoms, and Causes of Nerve Pain
Signs and Symptoms:
- Sharp, burning, or shooting pain
- Tingling or “pins and needles” sensation
- Numbness or reduced sensation
- Muscle weakness in the affected area
- Sensitivity to touch or temperature changes
- Pain that worsens at night
Causes:
- Injury: Trauma or compression of nerves, such as in carpal tunnel syndrome or sciatica.
- Diabetes: High blood sugar levels can damage nerves over time, leading to diabetic neuropathy.
- Infections: Shingles, HIV/AIDS, and Lyme disease can cause nerve damage and pain.
- Autoimmune Diseases: Conditions like multiple sclerosis and lupus can lead to nerve inflammation and pain.
- Chemotherapy: Certain cancer treatments can cause peripheral neuropathy, resulting in nerve pain.
Mechanism of Action of Muscle Pain & Nerve Pain
For Muscle Pain
Muscle pain, or myalgia, results from the activation of nociceptors, which are specialized nerve endings that detect damage or potential damage to tissues. Understanding this process involves several steps:
-
Activation of Nociceptors
Nociceptors in muscle tissue detect various types of stimuli:
- Mechanical Stress: Overuse, heavy lifting, or trauma can physically damage muscle fibers.
- Thermal Changes: Extreme temperatures can affect muscle cells.
- Chemical Stimuli: Substances released during tissue injury or inflammation can activate nociceptors.
-
Inflammatory Response
When muscle tissue is damaged, an inflammatory response occurs:
- Release of Inflammatory Mediators:
- Prostaglandins: These are produced at the site of injury and contribute to pain and inflammation.
- Bradykinin: This peptide causes blood vessels to dilate (expand), which increases blood flow and contributes to the sensation of pain.
- Cytokines: Small proteins like interleukins and tumor necrosis factor-alpha (TNF-α) help coordinate the inflammatory response.
These mediators sensitize nociceptors, making them more sensitive to stimuli that would not normally cause pain.
-
Transmission of Pain Signals
The process of transmitting pain signals involves several steps:
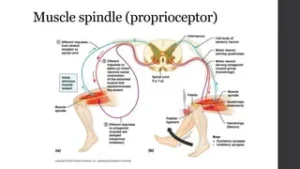
- Peripheral Nerves: Nociceptors send signals through peripheral nerves to the spinal cord.
- Spinal Cord: The spinal cord acts as a relay station, processing the pain signals and sending them to the brain via ascending pathways.
- Brain: Specific brain regions, including the thalamus and cerebral cortex, interpret these signals, leading to the conscious perception of pain.
-
Perception of Pain
The brain’s interpretation of pain signals is influenced by several factors:
- Thalamus: This part of the brain acts as a central relay for sensory information, including pain.
- Cerebral Cortex: Here, the brain interprets pain signals, which is where we become consciously aware of the pain.
- Influence of Psychological Factors: Emotional state, past experiences, and overall health can affect how pain is perceived.
-
Role of Pain in Healing
Pain serves as a protective mechanism:
- Promotes Rest: Pain encourages individuals to rest the injured area, preventing further damage.
- Inflammation and Healing: Although inflammation contributes to pain, it also brings immune cells and nutrients to the site of injury, promoting tissue repair.
Additional Details
- Muscle Spasm: In response to injury, muscles may spasm to protect the affected area, which can also contribute to pain.
- Secondary Hyperalgesia: Sometimes, the area surrounding an injury can become hypersensitive, a phenomenon known as secondary hyperalgesia, where even light touch can cause pain.
For Nerve Pain:
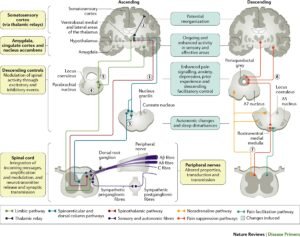
Nerve pain, or neuropathic pain, results from damage to or dysfunction of the nerves themselves, which can lead to abnormal signaling and pain perception. Understanding the mechanism of nerve pain involves several complex processes:
-
Nerve Damage or Dysfunction
Nerve pain can arise from various causes, such as:
- Injury: Trauma from accidents, surgeries, or medical procedures can damage nerves.
- Diseases: Conditions like diabetes, multiple sclerosis, and shingles can affect nerve function.
- Compression: Nerves can be compressed by tumors, herniated discs, or carpal tunnel syndrome.
- Infections: Infections such as HIV or Lyme disease can damage nerves.
-
Pathophysiological Changes in Nerves
When nerves are damaged, several pathological changes can occur:
- Axonal Damage: The nerve fibers (axons) can be damaged, leading to disrupted signal transmission.
- Demyelination: The protective myelin sheath around nerves can be damaged, impairing the speed and efficiency of electrical signal transmission.
-
Abnormal Electrical Activity
Damaged nerves can exhibit abnormal electrical activity:
- Ectopic Discharges: Nerve fibers may start to fire spontaneously without any external stimulus, leading to pain signals being sent to the brain.
- Hyperexcitability: Damaged nerves can become hyperexcitable, responding excessively to normal stimuli or even to stimuli that typically wouldn’t cause pain.
-
Sensitization
Sensitization plays a crucial role in nerve pain:
- Peripheral Sensitization: This occurs at the level of the damaged nerves. Inflammatory mediators and damaged nerve cells release substances that lower the threshold for pain signals, causing even minor stimuli to be perceived as painful.
- Central Sensitization: This occurs in the spinal cord and brain. Persistent nerve pain can cause changes in the central nervous system that amplify pain signals. This results in increased pain sensitivity and a lower threshold for pain.
-
Altered Pain Pathways
The way pain signals are processed and interpreted by the central nervous system changes in neuropathic pain:
- Increased Glutamate Activity: Enhanced release of the neurotransmitter glutamate can lead to heightened pain perception.
- Decreased Inhibitory Signals: Reduction in the normal inhibitory signals that would typically dampen pain perception can lead to an unregulated pain response.
-
Molecular and Cellular Mechanisms
Several molecular and cellular mechanisms contribute to nerve pain:
- Inflammatory Mediators: Cytokines, chemokines, and other inflammatory substances can directly sensitize nerve fibers.
- Ion Channel Changes: Changes in the expression and function of ion channels (such as sodium and calcium channels) in nerve membranes can lead to abnormal nerve firing.
- Neurotrophic Factors: Alterations in neurotrophic factors, which support nerve health, can contribute to nerve dysfunction and pain.
-
Pain Perception
The final stage involves the perception of pain by the brain:
- Thalamus: Acts as the relay center for sensory information, including pain.
- Somatosensory Cortex: Interprets pain signals, where the intensity and location of the pain are perceived.
- Emotional Response: Areas of the brain involved in emotional processing, such as the limbic system, also respond to pain, contributing to the emotional experience of pain.
Additional Details
- Pain Radiating: Neuropathic pain often radiates along the path of the affected nerve, leading to pain in areas not directly injured.
- Allodynia and Hyperalgesia: Individuals with nerve pain may experience allodynia (pain from non-painful stimuli) and hyperalgesia (increased sensitivity to painful stimuli).
Difference Between Muscle Pain & Nerve Pain
Understanding the differences between muscle pain and nerve pain is crucial for accurate diagnosis and effective treatment. Here are some key distinctions:
Origin
- Muscle Pain: Arises from muscle tissue, which includes muscles themselves, tendons, and ligaments.
- Nerve Pain: Originates from nerves, which can be peripheral nerves (outside the brain and spinal cord) or central nerves (within the brain and spinal cord).
Types of Pain
- Muscle Pain:
- Typically dull, aching, or throbbing.
- Can be localized to a specific area or muscle group.
- Often described as sore or stiff.
- Nerve Pain:
- Often sharp, burning, or shooting.
- Can be accompanied by a tingling or “pins and needles” sensation.
- May radiate along the path of the affected nerve, sometimes making it feel like it spreads from one area to another.
Associated Symptoms
- Muscle Pain:
-
- Swelling and redness around the affected area.
- Limited range of motion or stiffness in the affected muscle or joint.
- Muscle weakness or cramping.
- Tenderness when touching or pressing on the muscle.
- Nerve Pain:
-
- Tingling or numbness, especially in the extremities (hands and feet),.
- Hypersensitivity to touch or temperature changes (allodynia).
- Muscle weakness or paralysis in severe cases.
- Sudden, unexpected jolts of pain (electric shock-like sensations).
Response to Movement
- Muscle Pain:
-
- Generally, it worsens with movement or pressure on the affected muscle.
- Stretching or contracting the muscle may exacerbate the pain.
- Often relieved by rest and avoiding strenuous activity.
- Nerve Pain:
-
- Can be more unpredictable and may worsen with certain positions or activities.
- Often exacerbated at night or during rest periods,.
- May not necessarily improve with rest and can persist or worsen over time.
Duration and Onset
- Muscle Pain:
-
- Often acute, lasting a few days to a few weeks.
- It usually resolves with proper rest and treatment.
- Can become chronic if the underlying cause is not addressed.
- Nerve Pain:
-
- Can be chronic and persistent, lasting months to years.
- May have a gradual onset or develop suddenly.
- Often requires long-term management strategies.
Treatment Response
- Muscle Pain:
-
- Responds well to RICE (Rest, Ice, Compression, Elevation).
- Anti-inflammatory medications such as ibuprofen or naproxen can help reduce pain and swelling.
- Physical therapy exercises to strengthen muscles and improve flexibility.
- Massage and gentle stretching to relieve tension and improve blood flow.
- Nerve Pain:
-
- May require medications that target nerve function, such as anticonvulsants (e.g., gabapentin, pregabalin) or antidepressants (e.g., amitriptyline, duloxetine).
- Pain relievers like opioids or non-steroidal anti-inflammatory drugs (NSAIDs) may be less effective.
- Physical therapy techniques to improve nerve function and alleviate pressure on the affected nerve.
- Interventional procedures like nerve blocks or spinal cord stimulation for severe cases.
Diagnostic Tools
- Muscle Pain:
-
- Physical examination to assess muscle strength, flexibility, and tenderness.
- Imaging tests like X-rays, MRIs, or ultrasounds are used to detect muscle tears or inflammation.
- Blood tests to identify markers of inflammation or muscle damage.
- Nerve Pain:
-
- Neurological examination to assess sensation, reflexes, and motor function.
- Nerve conduction studies (NCS) and electromyography (EMG) are used to evaluate nerve function and detect abnormalities.
- Imaging tests like MRI or CT scans are used to identify structural issues that are compressing or damaging nerves.
- Blood tests to rule out underlying conditions like diabetes or vitamin deficiencies.
Causes
- Muscle Pain:
-
- Overuse or strain from physical activity.
- Direct injury or trauma.
- Muscle tension or stress.
- Medical conditions like fibromyalgia or myositis.
- Nerve Pain:
-
- Nerve compression from conditions like herniated discs or carpal tunnel syndrome.
- Nerve damage from diabetes (diabetic neuropathy).
- Infections such as shingles (postherpetic neuralgia) or HIV.
- Autoimmune diseases like multiple sclerosis.
Psychological Impact
- Muscle Pain:
-
- Can lead to frustration or anxiety, especially if it limits daily activities.
- Generally, it has a lower impact on mental health compared to nerve pain.
- Nerve Pain:
-
- Often associated with significant psychological distress, including anxiety and depression.
- Chronic nature and severity can severely impact quality of life and mental health.
Prognosis
- Muscle Pain:
-
- Typically has a good prognosis with proper treatment and rest.
- Most acute muscle pains resolve completely.
- Nerve Pain:
-
- Often requires long-term management.
- Prognosis depends on the underlying cause and the effectiveness of treatment strategies.
- May lead to chronic pain conditions if not properly managed.
Recognizing and Diagnosing Muscle Pain & Nerve Pain
Accurate diagnosis of muscle and nerve pain involves a comprehensive approach, including:
Patient History
- Detailed Questioning: Gathering a comprehensive patient history is the first step in diagnosing muscle and nerve pain. The healthcare provider will ask about:
- Onset of Pain: When did the pain start?
- Nature of Pain: How does the pain feel (e.g., sharp, dull, throbbing, burning)?
- Duration of Pain: Is the pain constant or intermittent?
- Associated Symptoms: Are there any additional symptoms, such as swelling, redness, tingling, or numbness?
- Potential Triggers: What activities or conditions seem to trigger or worsen the pain (e.g., physical activity, rest, certain positions)?
- Previous Medical History: Any history of injuries, surgeries, or chronic conditions that might be related to the pain.
- Lifestyle Factors: Work habits, physical activity levels, and any recent changes in activity or stress levels.
Physical Examination
- Assessment of Muscle Strength: The provider will test the strength of various muscle groups to identify any weakness or imbalance.
- Joint Function Evaluation: Assessing the range of motion in the joints can help determine if the pain is related to joint issues.
- Palpation for Tenderness: The provider will feel the muscles and joints to identify areas of tenderness, swelling, or deformity.
- Neurological Examination: Testing reflexes, sensation, and motor function can help distinguish between muscle and nerve pain.
Diagnostic Tests
- Imaging Studies:
- X-rays: Useful for detecting bone fractures, joint space narrowing, and osteoarthritis, which can contribute to muscle and nerve pain.
- Magnetic Resonance Imaging (MRI): Provides detailed images of soft tissues, including muscles, tendons, ligaments, and nerves. MRI can identify conditions like herniated discs, muscle tears, and nerve compression.
- Computed Tomography (CT) Scans: Offers cross-sectional images of the body and is useful for detecting bone abnormalities and a detailed assessment of certain conditions affecting muscles and nerves.
- Electromyography (EMG) and Nerve Conduction Studies:
- EMG: Measures the electrical activity of muscles at rest and during contraction. It helps diagnose muscle disorders and conditions that affect the connection between nerves and muscles.
- Nerve Conduction Studies: Measure how well and how fast nerves can send electrical signals. This test is essential for diagnosing nerve damage and identifying the specific nerves affected.
- Blood Tests:
- Markers of Inflammation: Tests like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) can indicate inflammation.
- Infections and Autoimmune Diseases: Blood tests can rule out infections or autoimmune conditions that might cause or contribute to pain (e.g., rheumatoid arthritis, lupus).
- Metabolic Disorders: Tests to check for diabetes, thyroid function, and other metabolic issues that can affect muscles and nerves.
Recognizing Muscle Pain
- Pain Characteristics: Dull, aching, or throbbing pain that is usually localized to a specific area.
- Trigger Points: Specific spots within the muscle that are tender to touch and can trigger pain elsewhere in the body.
- Muscle Weakness: Decreased strength in the affected muscle.
- Swelling and Redness: Possible signs of inflammation or injury.
Recognizing Nerve Pain
- Pain Characteristics: Sharp, burning, or shooting pain that can radiate along the path of a nerve.
- Tingling and Numbness: Often experienced in the extremities (hands and feet).
- Hypersensitivity: Increased sensitivity to touch, temperature changes, or other stimuli.
- Motor Dysfunction: Muscle weakness or paralysis in severe cases of nerve damage.
Physiotherapy Treatment and Intervention Exercises for Muscle and Nerve Pain
For Muscle Pain:
- Stretching Exercises:
- Hamstring Stretch: Improves flexibility in the back of the thigh.
- Quadriceps Stretch: Targets the front of the thigh.
- Calf Stretch: Enhances flexibility in the lower leg.
- Shoulder Stretch: Relieves tension in the shoulder muscles.
- Back Stretch: Eases tension in the lower back.
- Strengthening Exercises:
- Leg Press: Strengthens quadriceps and gluteal muscles.
- Hamstring Curls: Targets the back of the thigh.
- Bicep Curls: Strengthens arm muscles.
- Shoulder Press: Enhances shoulder muscle strength.
- Core Strengthening (Planks, Bridges): Improves core stability and strength.
- Aerobic Exercises:
- Walking: Improves overall cardiovascular fitness and reduces muscle stiffness.
- Swimming: Low-impact exercise that enhances muscle strength and flexibility.
- Cycling: Strengthens leg muscles and improves joint mobility.
- Electrotherapy:
- TENS (Transcutaneous Electrical Nerve Stimulation): Relieves pain by stimulating nerves.
- Ultrasound Therapy: Promotes tissue healing and reduces inflammation.
- Interferential Therapy (IFT): Reduces pain and muscle spasms through electrical stimulation.
For Nerve Pain:
- Nerve Gliding Exercises:
- Median Nerve Glide: Reduces tension in the median nerve.
- Ulnar Nerve Glide: Targets the ulnar nerve in the arm.
- Sciatic Nerve Glide: Eases tension in the sciatic nerve.
- Strengthening and Conditioning:
- Resistance Band Exercises: Improves overall muscle strength and supports nerve health.
- Core Strengthening: Planks, side planks, and bird-dog exercises enhance core stability.
- Stretching:
- Piriformis Stretch: Reduces sciatic nerve compression.
- Hip Flexor Stretch: Relieves tension in the hip area.
- Electrotherapy:
- TENS: Provides pain relief by blocking nerve signals.
- Electromyostimulation (EMS): Enhances muscle strength and function through electrical impulses.
- Laser Therapy: Reduces inflammation and promotes nerve healing.
Home Exercises:
- Advantages of Home Exercises:
- It is convenient and can be done at any time
- Cost-effective
- Empowers patients to take control of their rehabilitation
- Consistent practice can lead to better outcomes
- Examples of Home Exercises:
- Foam Rolling: Relieves muscle tension and improves blood flow.
- Heel Slides: Enhances knee mobility and strength.
- Pelvic Tilts: Strengthens the lower back and abdominal muscles.
- Wall Slides: Improves shoulder mobility and strength.
- Ankle Pumps: Reduce swelling and enhance circulation in the legs.
Prognosis
The prognosis for muscle and nerve pain varies depending on the underlying cause, the severity of the condition, and the effectiveness of the treatment plan. With appropriate diagnosis and comprehensive physiotherapy intervention, many patients experience significant improvement in pain relief, mobility, and overall quality of life. Chronic conditions may require long-term management strategies to maintain optimal function and prevent recurrence.
Conclusion
Muscle pain and nerve pain, while often presenting with similar symptoms, are fundamentally different in their origins, mechanisms, and treatments. Accurate diagnosis and a tailored physiotherapy approach are essential for effective management. By understanding the nuances of each type of pain and implementing appropriate interventions, physiotherapists can help patients achieve significant pain relief, improved function, and an enhanced quality of life. Regular exercise, both in clinical settings and at home, plays a crucial role in maintaining joint and muscle health, ultimately leading to better outcomes for individuals suffering from muscle and nerve pain.
