Osteoarthritis: A Biological Guide!
Anatomy of Osteoarthritis
Osteoarthritis (OA) is a degenerative joint disease characterized by the breakdown of cartilage in the joints. Joint pain typically marks the onset of morbidity in osteoarthritis, characterized by a deep, achy sensation in the joints that worsens with prolonged activity. Additionally, individuals commonly experience a decrease in range of motion and may notice a grinding or crackling sensation within the joint, known as crepitus. Stiffness, particularly upon waking (known as gelling), can also develop, typically lasting for less than half an hour in the morning.
Understanding the anatomy of the affected joints is crucial for comprehending how osteoarthritis develops and progresses.
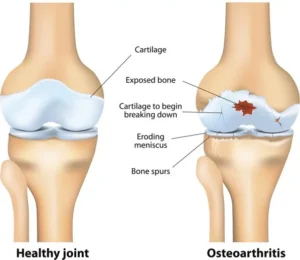
In a healthy joint, several components work together to facilitate smooth movement and provide stability. These components include:
- Cartilage: A smooth, rubbery tissue that covers the ends of bones where they meet to form a joint. Cartilage acts as a cushion, absorbing shock and reducing friction during movement.
- Synovium: A thin membrane that lines the joint capsule and produces synovial fluid. Synovial fluid lubricates the joint, nourishes the cartilage, and helps reduce friction between the joint surfaces.
- Joint Capsule: A tough, fibrous structure that surrounds the joint and helps hold it together. The joint capsule contains the synovium and provides stability to the joint.
- Ligaments: Strong bands of connective tissue that connect bones to each other and help stabilize the joint.
- Tendons: Fibrous cords that connect muscles to bones and help control movement of the joint.
In osteoarthritis, the cartilage in the joint undergoes degenerative changes, becoming thin, frayed, and eventually worn away. This results in the bones rubbing against each other, causing pain, swelling, and stiffness.
Physiology of Osteoarthritis
The physiology of OA involves complex interactions between various factors, including mechanical stress, inflammation, and biochemical changes within the joint. Mechanical stress, such as repetitive joint loading or injury, plays a significant role in initiating and exacerbating OA. This stress can lead to microtrauma and damage to the articular cartilage, triggering an inflammatory response.
Pro-inflammatory cytokines, such as interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-α), drive inflammation in OA by releasing them. These cytokines contribute to cartilage degradation and joint damage. Chondrocytes, responsible for maintaining cartilage, respond to inflammation by undergoing metabolic changes. This response leads to an increase in the production of matrix-degrading enzymes and a decrease in the synthesis of extracellular matrix components.
Progressive cartilage loss and structural changes within the joint, including osteophyte formation, subchondral bone sclerosis, and synovial inflammation, result from the imbalance between cartilage degradation and repair processes. These changes further contribute to joint pain, stiffness, and functional impairment in OA patients.
Pathophysiology of Osteoarthritis
The pathophysiology of OA involves a complex interplay of mechanical, biochemical, and genetic factors that contribute to joint degeneration. While the exact mechanisms underlying OA development are not fully understood, several key processes have been identified.
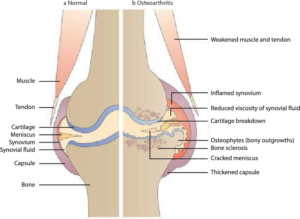
- Cartilage Degradation: The primary feature of OA is the progressive breakdown of articular cartilage, resulting in the loss of its smooth surface and structural integrity. The increased activity of matrix metalloproteinases (MMPs) and aggrecanases drives this process, as these enzymes degrade cartilage matrix components.
- Subchondral Bone Changes: Subchondral bone undergoes remodeling in response to altered mechanical loading and cartilage damage in OA. This remodeling is characterized by increased bone density (sclerosis), the formation of osteophytes (bone spurs), and subchondral cysts.
- Synovial Inflammation: Inflammation of the synovial membrane (synovitis) is a common feature of OA, contributing to joint pain and swelling. Synovial inflammation is mediated by pro-inflammatory cytokines, chemokines, and immune cells infiltrating the joint space.
- Ligament and Tendon Involvement: Ligaments and tendons surrounding the affected joint may undergo structural changes and degeneration in OA. This can lead to joint instability and further compromise joint function.
Etiology of Osteoarthritis
The etiology of osteoarthritis is multifactorial, with both genetic and environmental factors contributing to disease development. While the exact cause of osteoarthritis remains elusive, several key etiological factors have been identified:
- Age: Osteoarthritis is more common in older adults, with age-related changes in cartilage structure and function contributing to disease progression.
- Genetics: Genetic factors play a significant role in determining an individual’s susceptibility to osteoarthritis. Variations in genes encoding cartilage matrix proteins, enzymes involved in cartilage metabolism, and inflammatory mediators can influence disease risk.
- Obesity: Excess body weight is a major risk factor for osteoarthritis, particularly in weight-bearing joints such as the knees and hips. Obesity increases joint loading and contributes to cartilage wear and tear.
- Joint Injury: Previous joint injuries, such as fractures, ligament tears, or repetitive stress injuries, can predispose individuals to osteoarthritis later in life.
- Occupational Factors: Jobs that involve repetitive movements, heavy lifting, or prolonged standing can increase the risk of osteoarthritis, particularly in the joints of the hands, knees, and spine.
Does Nerve Damage Cause Osteoarthritis?
While nerve damage itself does not directly cause OA, it can contribute to the development and progression of the disease. Nerve damage in OA is often secondary to joint inflammation, mechanical stress, or structural changes within the joint. Chronic joint pain and inflammation associated with OA can lead to nerve sensitization and neuropathic pain, further exacerbating symptoms and functional impairment.

How Does Nerve Damage Occur in Osteoarthritis?
Nerve damage in OA can occur through several mechanisms:
- Inflammatory Mediators: Inflammatory cytokines released during joint inflammation can directly affect nerve fibers, leading to sensitization and hyperexcitability. These cytokines can also induce the expression of pain-related receptors on nerve cells, increasing their responsiveness to pain stimuli.
- Mechanical Compression: Structural changes within the joint, such as osteophyte formation or synovial proliferation, can compress nearby nerves, leading to nerve entrapment and neuropathic pain. Mechanical compression can also disrupt nerve function and impair nerve signaling.
- Neurovascular Changes: Alterations in local blood flow and vascular permeability in OA joints can compromise nerve health and function. Reduced blood flow to nerves can deprive them of oxygen and nutrients, leading to nerve degeneration and dysfunction.
- Central Sensitization: Chronic pain and inflammation in OA can trigger changes in the central nervous system, leading to central sensitization. This process involves the amplification of pain signals within the spinal cord and brain, resulting in heightened pain perception and sensitivity to stimuli.
In conclusion, while nerve damage does not directly cause OA, it can contribute to pain and functional impairment in affected individuals.
Conclusion
Osteoarthritis is a complex and multifaceted disease characterized by the progressive degeneration of joint tissues. Understanding the anatomy, physiology, pathophysiology, and etiology of osteoarthritis is essential for developing effective prevention and treatment strategies. While nerve damage itself does not directly cause osteoarthritis, it can contribute to pain and disability in affected individuals. Further research into the mechanisms of nerve damage in osteoarthritis is needed to identify novel therapeutic targets and improve patient outcomes.

Pingback: Osteoarthritis: A Physio Guide! - Azmi Writes & Creates
With your post, your readers, particularly those beginners who are trying to explore this field won’t leave your page empty-handed. Here is mine at Article Star I am sure you’ll gain some useful information about SEO too.