Osteoarthritis: In-Depth Guide!
Overview
Osteoarthritis (OA) is a degenerative joint disease characterized by the breakdown of cartilage, the smooth tissue that cushions the ends of bones in joints. This condition leads to pain, stiffness, swelling, and a decreased range of motion. OA is the most common form of arthritis, affecting millions of people worldwide. It typically affects joints that bear weight, such as the knees, hips, and spine, but it can also impact the hands and other joints. The progression of OA can vary from person to person, with some experiencing mild symptoms and others facing significant disability.

History
The understanding and recognition of osteoarthritis date back to ancient times. Evidence of OA has been found in the skeletal remains of prehistoric humans, suggesting that this condition has afflicted humans for millennia. The term “osteoarthritis” itself is derived from Greek words: “osteon,” meaning bone, “arthron,” meaning joint, and “itis,” indicating inflammation.
Historically, OA was often referred to as “degenerative arthritis” or “degenerative joint disease.” In the 19th century, physicians began to distinguish OA from other forms of arthritis, such as rheumatoid arthritis, based on clinical and pathological features. Sir Alfred Garrod, an English physician, played a significant role in differentiating OA from other rheumatic diseases in the late 1800s. His work laid the foundation for the modern understanding of OA as a distinct clinical entity.
Advances in medical imaging, particularly X-rays in the early 20th century, allowed for better visualization of joint changes associated with OA. This development further refined the diagnosis and classification of the disease. Over the years, research has expanded our knowledge of the biochemical and biomechanical processes underlying OA, leading to more targeted approaches for its management and treatment.
Causes of Osteoarthritis
The exact cause of osteoarthritis is not fully understood, but it is believed to result from a combination of genetic, mechanical, and environmental factors. Some of the primary causes include:
- Mechanical Stress: Repeated stress or injury to the joint can damage cartilage and contribute to the development of OA. This is common in athletes and individuals whose occupations involve repetitive joint movements or heavy lifting.
- Aging: The risk of developing OA increases with age. As people age, the cartilage becomes more brittle and less able to repair itself.
- Genetics: Certain genetic factors may predispose individuals to OA. For instance, some people inherit defects in the genes responsible for cartilage production and maintenance.
- Inflammation: Chronic low-level inflammation can contribute to the breakdown of cartilage.
- Biochemical Changes: Changes in the composition and function of cartilage cells (chondrocytes) and the extracellular matrix can lead to cartilage degradation.
Risk Factors of Osteoarthritis
Several factors increase the risk of developing osteoarthritis, including:
- Age: The risk of OA increases significantly with age.
- Gender: Women are more likely to develop OA, particularly after menopause.
- Obesity: Excess body weight increases the stress on weight-bearing joints, such as the knees and hips.
- Joint Injuries: Injuries from sports, accidents, or repetitive use can increase the risk of OA in the affected joints.
- Genetics: A family history of OA can increase an individual’s risk.
- Bone Deformities: Some people are born with malformed joints or defective cartilage, which can lead to OA.
- Occupation: Jobs that involve repetitive stress on specific joints can increase the risk of OA.
Signs of Osteoarthritis
The signs of osteoarthritis can vary depending on the severity and location of the disease. Common signs include:
- Joint pain: Pain in the affected joint(s) during or after movement.
- Stiffness: Joint stiffness, especially in the morning or after periods of inactivity.
- Swelling: Swelling around the joint, caused by inflammation and excess synovial fluid.
- Loss of Flexibility: Decreased range of motion in the affected joint.
- Grating Sensation: A sensation of grating or bone rubbing against bone.
- Bone Spurs: Hard lumps around the joint, which are bone growths (osteophytes).

Symptoms of Osteoarthritis
The symptoms of osteoarthritis often develop gradually and worsen over time. Key symptoms include:
- Pain: Persistent or intermittent joint pain, which may worsen with activity and improve with rest.
- Tenderness: The joint may feel tender when pressed.
- Stiffness: Joint stiffness, particularly after waking up or being inactive for a prolonged period.
- Swelling: Swelling and inflammation in the affected joint.
- Reduced Range of Motion: Difficulty moving the joint through its full range of motion.
- Creaking or Grating Sensation: A sensation of the joint creaking, crackling, or grinding during movement.
- Loss of Function: Severe OA can lead to significant disability and loss of function in the affected joint.
Affected Body Parts and Percentages
Osteoarthritis can affect any joint, but it most commonly impacts the following areas:
- Knees (45–60%): The knees are the most commonly affected joints due to their role in weight-bearing and movement.
- Hips (20–30%): The hips are also frequently affected, leading to pain and stiffness in the groin, thigh, or buttock.
- Hands (10–20%): OA in the hands often affects the base of the thumb, the fingertips, and the middle joints of the fingers.
- Spine (10–20%): The cervical (neck) and lumbar (lower back) regions of the spine are commonly affected, causing pain and stiffness in these areas.
- Feet (5–10%): The joints at the base of the big toe are often affected, leading to pain and swelling.
Potential Consequences
If left untreated, osteoarthritis can lead to several serious complications, including:
- Chronic Pain: Persistent pain can significantly impact an individual’s quality of life and lead to emotional and psychological distress.
- Disability: Severe OA can result in a significant disability, limiting a person’s ability to perform daily activities and reducing their independence.
- Joint Deformities: Progressive damage to the joint can cause deformities, such as bowlegged or knock-kneed appearances.
- Reduced Mobility: Decreased range of motion and joint stiffness can make it difficult to move around and perform everyday tasks.
- Secondary Conditions: OA can lead to other health issues, such as muscle weakness, poor balance, and an increased risk of falls.
Stages of Osteoarthritis
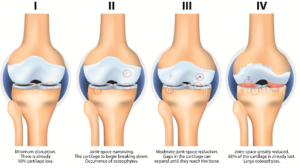
Osteoarthritis progresses through several stages, each with distinct characteristics:
- Stage 1 (minor): Minimal wear and tear in the joints, with little to no pain.
- Stage 2 (Mild): Noticeable bone spurs and joint pain after long periods of activity. Cartilage begins to break down.
- Stage 3 (Moderate): Erosion of cartilage leads to joint stiffness and swelling. Pain becomes more frequent and severe.
- Stage 4 (Severe): Significant loss of cartilage, with large bone spurs and severe pain. Joint space is greatly reduced, leading to limited mobility and significant disability.
Classification of Osteoarthritis
Osteoarthritis can be classified based on its cause, location, and severity:
- Primary Osteoarthritis: This form of OA develops without any apparent underlying cause, often associated with aging and genetic predisposition.
- Secondary Osteoarthritis: This type of OA is caused by another condition or factor, such as joint injury, obesity, or other diseases like rheumatoid arthritis or gout.
Based on the location of the affected joints, OA can be further classified as:
- Localized OA: Affecting one or a few joints.
- Generalized OA: Affecting multiple joints throughout the body.
Severity-based classification includes:
- Mild OA: Minor symptoms with minimal impact on daily activities.
- Moderate OA: More noticeable symptoms that interfere with daily activities.
- Severe OA: Severe symptoms leading to significant disability and reduced quality of life.
Conclusion
Osteoarthritis is a prevalent and debilitating joint disease that affects millions of people worldwide. Understanding its causes, risk factors, and symptoms is crucial for early diagnosis and effective management. While there is currently no cure for OA, various treatments and lifestyle modifications can help manage symptoms and improve quality of life. Research continues to advance our understanding of OA, offering hope for more effective therapies and potentially even preventive measures in the future.

Pingback: Osteoarthritis: A Biological Guide! - Azmi Writes & Creates
Hey there, I love all the points you made on that topic. There is definitely a great deal to know about this subject, and with that said, feel free to visit my blog Webemail24 to learn more about Data Mining.
This is quality work regarding the topic! I guess I’ll have to bookmark this page. See my website Seoranko for content about Rental Car Services and I hope it gets your seal of approval, too!